How health insurance coverage impacts access to children's mental health care

SeventyFour // Shutterstock
How health insurance coverage impacts access to children’s mental health care
Psychologist taking notes in therapy session.
Emergency rooms see almost half a million chidren per year for mental health conditions, according to the American Academy of Pediatrics—and that number has been growing.
Children ages 6 to 17 have an increasing need for mental health services, with 1 in 6 reporting at least one mental health disorder, according to a 2019 paper from researchers at the University of Michigan. And that was before the COVID-19 pandemic, which hit children’s mental health hard. High school students are increasingly reporting persistent feelings of sadness or hopelessness. According to the Centers for Disease Control and Prevention’s Youth Risk Behavior Survey, 42% of high school students experienced these feelings in 2021, an increase of five percentage points from 2019 and 14 points higher than in 2011.
However, about half of youth who need professional mental health services don’t get it, according to the same Michigan researchers. Among the barriers to accessing mental health care for children: health insurance coverage.
CounselingSchools.com explored how insurance doesn’t guarantee mental health coverage, and the differences for youth covered by Medicaid versus private plans, incorporating Kaiser Family Foundation data.
Getting children the help they need covered by insurance can be tough for parents, even with the laws requiring parity in mental and physical health coverage. Historically, health insurers offered little in the way of mental health benefits. In 1996, a federal law introduced the idea of covering mental health to the same degree as physical health services, but not for all health plans. That concept expanded with the Mental Health Parity and Addiction Equity Act of 2008, which required insurers to treat mental and physical health coverage similarly.
That said, NPR has reported that insurance companies tend to be lax about ensuring equal coverage for mental health care, often treating mental illness as an acute condition instead of a chronic condition that may require longer-term care.
The laws apply to most health plans, but there are several types of exceptions, the Kaiser Family Foundation reports. NPR reports one example where a family in Ohio had to pay $40,000 out-of-pocket for their daughter’s residential treatment for chronic suicidality after their insurer halted coverage. The family eventually got through the red tape to continue treatment and get reimbursed for their expenses.
Schools try to provide support because untreated mental health conditions can hurt students’ learning and development. The Substance Abuse and Mental Health Services Administration found in 2019 that 15% of adolescents received mental health services at school. But that’s not enough to meet the need.
![]()
CounselingSchools.com
How mental health coverage for children on Medicaid differs from those on private insurance
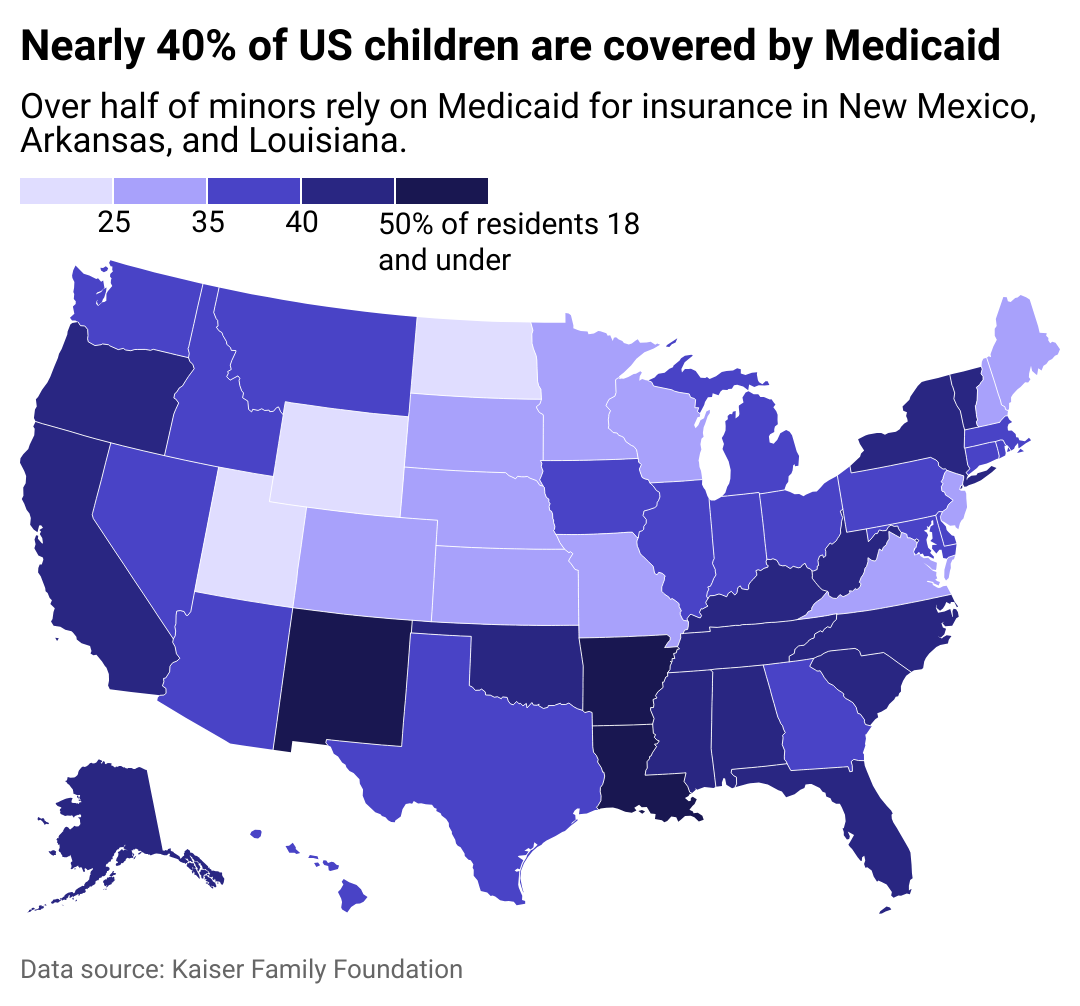
Map showing nearly 40% of US children are covered by Medicaid. Over half of minors rely on Medicaid for insurance in New Mexico, Arkansas, and Louisiana.
Medicaid and the Children’s Health Insurance Program, or CHIP, provide youth up to age 21 on Medicaid and age 19 on CHIP with a wide range of comprehensive services for mental health through the Early and Periodic Screening, Diagnostic, and Treatment benefit, according to KFF.
Under that benefit, young people can receive screenings for mental health, behavioral health, and developmental issues—along with physical health screenings—and obtain any services necessary to treat any mental and behavioral diagnosis, even if a state Medicaid program doesn’t cover the service. According to The Commonwealth Fund, the benefit allows youth on Medicaid to get better, more complete mental health services than youth covered by commercial insurance.
Many states are using Medicaid programs to reach children through school services—21 states have laws extending Medicaid to cover school-based health care, including mental health services. For example, youth covered by Medicaid in Colorado may access mental health services without a formal diagnosis, which allows for more early intervention, according to an Education Week report.
Story editing by Jeff Inglis and Kelly Glass. Copy editing by Tim Bruns.
This story originally appeared on CounselingSchools.com and was produced and
distributed in partnership with Stacker Studio.
