Hospital workers are working longer hours—here's how their time compares to other health care workers
Canva
Hospital workers are working longer hours—here’s how their time compares to other health care workers
A worker in green scrubs walks down a hospital hallway pushing an IV bag.
2023 was a year of historic labor action for U.S. health care workers. A three-day strike involving more than 75,000 Kaiser Permanente employees became the largest-ever documented health care strike in the U.S. The workers said their wages did not adjust for mounting rates of inflation and staffing levels were inadequate.
Doctors and medical residents have not historically unionized in the U.S. But, in 2023, a collection of 550 health care workers employed by the Allina Health System and based in Minneapolis became one of the country’s largest private-sector physician unions. From January 2021 to early November 2023, workers in the health care and social assistance sector staged 109 strikes, with a growing number each year. It’s a building trend in the U.S., though medical-sector strikes are much more common abroad.
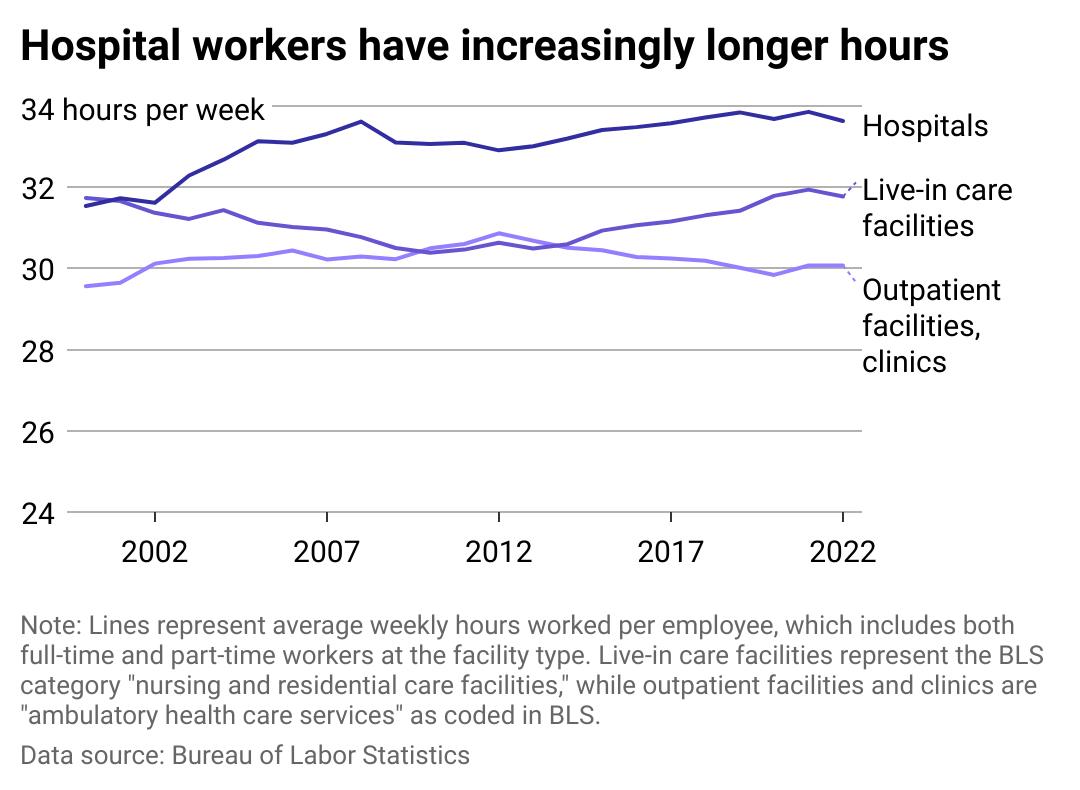
Incredible Health used Bureau of Labor Statistics data to analyze the change in weekly working hours among various health care industry workers.
A 2023 Tebra survey peeled back the curtain on health care workers’ consternation: 7 in 10 health care workers described their current workload and stress as untenable. Understaffing, burnout, and heavy administrative workloads are among the main reasons health care workers are protesting so fervently.
Still recovering from the effects of the pandemic
The health care system has yet to rebound from the stressors of the COVID-19 pandemic, when many workers left the industry, worsening an existing staffing shortfall.
In 2020, an Association of American Medical Colleges report estimated that the demand for physicians will outpace supply—snowballing into a shortage of 54,100 to 139,000 physicians by 2033, with the biggest shortages in primary care and rural communities.
However, a study published in November 2023 by the Journal of the American Medical Association, around the announcement of President Joe Biden’s proposed nursing home staffing requirement, shows that while some staffing levels had almost rebounded to pre-pandemic levels by the end of 2022, the effects of COVID-19 to staffing levels in nursing facilities is still profound. Nursing facility staff numbers are 10.5% lower than pre-pandemic and skilled nursing facility staffing is 12% lower.
Overloaded health care staff are roughly twice as likely to leave their jobs than workers who report not being overloaded, according to a study published in the Journal of General Internal Medicine in March 2023.
Burnout is so widespread in health care that the U.S. surgeon general issued an advisory during the pandemic to call attention to the well-being of health workers. The World Health Organization’s definition of burnout is “an occupational syndrome resulting from chronic workplace stress due to an imbalance between job demands and resources,” which contributes to “reduced professional efficacy,” among other side effects.
Tebra’s 2023 survey of medical professionals found that more than 1 in 3 health care workers have made a mistake while working because of a lack of sleep, with 82% saying that patient care suffers the most when the workers are fatigued.
![]()
Incredible Health
Average hospital workers work longer hours, and their lead has grown
A multiline chart showing the average hours worked by employees in three separate health care industries: hospitals, live-in care facilities, and outpatient facilities and clinics.
Nursing home facilities are operating with the leanest workforce in health care right now, but BLS data shows that a smaller number of workers are still working roughly the same average number of weekly hours as a much larger workforce did in 2000.
The average ambulatory health care service professional’s hours have increased by half an hour a week to cover staff shortages in other parts of health care: Hospital workers are working two hours more a week.
Unlike other industries like airline pilots, where exhaustion and workload are under close watch, research shows that efforts to reduce workload in medicine are “haphazard” and mainly focused on trainees, according to the March 2023 paper published in the Journal of General Internal Medicine.
For emergency medical services professionals, 40-plus-hour workweeks are by necessity—for the workers, not for the patients. Research published in PubMed in 2020 shows that 71% of surveyed EMS professionals had to work overtime, or multiple jobs, to make ends meet.
Three-quarters of hospital nurses work 12-hour shifts, not including commute time, according to the American Nurses Association, since their schedules are based on around-the-clock patient care in hospitals and long-term care facilities.
Over the course of two years, around half of the nursing staff in Katie Carroll’s nursing unit at a hospital in New Brunswick, New Jersey, left, she told The New York Times. The effects of staff shortages can reverberate into patient care: “You’re running around so busy with a frazzled mind that more mistakes can happen, because there’s so much on your plate” Caroll said.
The consequences of overworked staff can be devastatingly fatal. Research published in 2021 by BMJ Open found that the probability of the 30-day mortality rate for a patient increased by 16% when an additional patient was added to the caseload of an average hospital nurse.
For physicians in 2021, the average workweek was 50 to 59 hours, though 36% worked 60 to 80 hours or more. Some of that is because of the corporate consolidation of U.S. health care. That activity, plus increased demands by insurers and hospital administrators, has led to “doctors drowning in a sea of paperwork and patient visits,” Dr. Robert Pearl, a former CEO of Permanente Medical Group, wrote for Forbes.
Even with so much on the shoulders of health care staff, many take on even more. The Accreditation Council for Graduate Medical Education has periodically proposed tighter restrictions than its 2003 limitations that capped medical residents’ work hours at 80 hours per week.
The Biden administration’s proposal to establish staffing minimums at nursing homes could also meaningfully clarify the 1987 act that simply required nursing homes to have “sufficient” staffing. That change could ensure nurses aren’t overworked, but the bill’s fate is in the air, facing significant criticism.
Hope might also come in the form of increased transparency during the hiring process. A March 2023 op-ed in Medical Economics argues that hourly pay transparency is becoming an expectation on job listings as clinicians want more information upfront.
Also, 77,000 health care jobs were created in November 2023, mostly in ambulatory health care services, hospitals, and nursing care facilities. If filled, the additional help could reduce the burden on other health care workers. But the need will continue to be significant.
Story editing by Jeff Inglis. Copy editing by Kristen Wegrzyn.
This story originally appeared on Incredible Health and was produced and
distributed in partnership with Stacker Studio.

