The US eliminated malaria in 1951. How can it keep it under control now?
Malaria was eliminated in the United States in 1951
By Meg Tirrell, CNN
(CNN) — Working underground in a Biosafety Level 3 insectary in Tres Cantos, Madrid, researchers at the pharmaceutical giant GSK were frustrated.
The mosquitoes they were using to study experimental medicines for malaria had developed a pesky problem: They were becoming resistant to the parasite, plasmodium, that causes the ancient disease.
“We needed to get this testing up and running as soon as possible,” said Dr. Janneth Rodrigues, GSK’s scientific leader of global health medicines research and development. “So we tried to find out the reasons for this loss of susceptibility.”
It turned out that the mosquitoes harbored a bacteria that secreted a chemical that inhibits development of the parasites. That meant the team had to shut the colony down for the purposes of research into new malaria drugs — but it also led them to a new potential way to combat malaria.
The finding, published this month in the journal Science, is now being tested further in field studies in Burkina Faso, Rodrigues said. The hope is that the bacteria, Delftia tsuruhatensis TC1, could one day become a “tool for potential use in conjunction with existing strategies to achieve global malaria eradication,” she and her co-authors wrote in their paper in Science.
The approach is one of several new technologies being developed in humanity’s centuries-long battle with mosquito-borne diseases. Other recent approaches include genetically modifying the bugs so they can’t produce viable offspring or even programming them with a technology known as a gene drive that would wipe out their entire population.
New tools are needed. Malaria kills an estimated 600,000 people every year, mainly young children in countries in Africa, where the disease is endemic. It’s so hard to fight there, says the National Institutes of Health’s Dr. Carolina Barillas-Mury, the burden of disease is hard to imagine for people who don’t experience it.
“In the highly endemic areas, when the rainy season comes, the infection rate is 300%,” said Barillas-Mury, chief of the Laboratory of Malaria and Vector Research at the National Institute of Allergy and Infectious Diseases. That means “everyone in that town will get three episodes of malaria every year. … You cure a group, and then the other ones get infected. It never ends.”
It’s a different story in countries like the United States, the reason that reports of eight cases of locally acquired malaria here this summer, the first in two decades, brought reassurances from public health officials.
“The risk is very low,” Dr. Peter McElroy, chief of the malaria branch in the US Centers for Disease Control and Prevention’s Division of Parasitic Diseases and Malaria, told CNN. Those cases, flagged in June, haven’t led to broader spread, McElroy pointed out.
On Friday, a separate locally acquired case was identified in Maryland. The new case involves the parasite Plasmodium falciparum, which can cause more severe illness than the strain in the Florida and Texas cases, P. vivax.
The numbers in the US weren’t always so low.
In 1935, McElroy said, there were 100,000 malaria cases in the US. In an effort to limit its impact in the southeastern US during World War II, particularly around military training bases, the US created the Office of Malaria Control in War Areas in 1942.
Later, that became the Communicable Disease Center, the precursor to today’s CDC. As the South had the most malaria transmission, the center was based in Atlanta, still home to the CDC today.
The tools used to control it now, while improved, adhere to many of the same principles.
The work then “focused on both prevention and treatment,” McElroy said, “because we wanted the program to address both mosquitoes and the parasite.”
Prevention efforts included draining standing bodies of water to eliminate places where mosquitoes breed and providing screens for people’s homes, said Dr. Daniel Markowski, technical adviser to the American Mosquito Control Association. The US eliminated malaria in 1951.
“What they were able to do in the late 1940s and ’50s was suppress the population so low that they could no longer effectively transmit malaria,” Markowski said. “But they didn’t eradicate all the Anopheles mosquitoes.”
More than 200 kinds of mosquitoes live in the continental US, according to the CDC, and about 12 carry germs that can make people sick. Many have different characteristics: where they breed, when they come out to bite and how far they can travel.
Anopheles, which carry the parasite that causes malaria, tend to be “very prolific, very aggressive human biters,” Markowski said. They’re found across the US, feeding at dusk and dawn, sometimes able to travel even miles per day to find a meal, he explained.
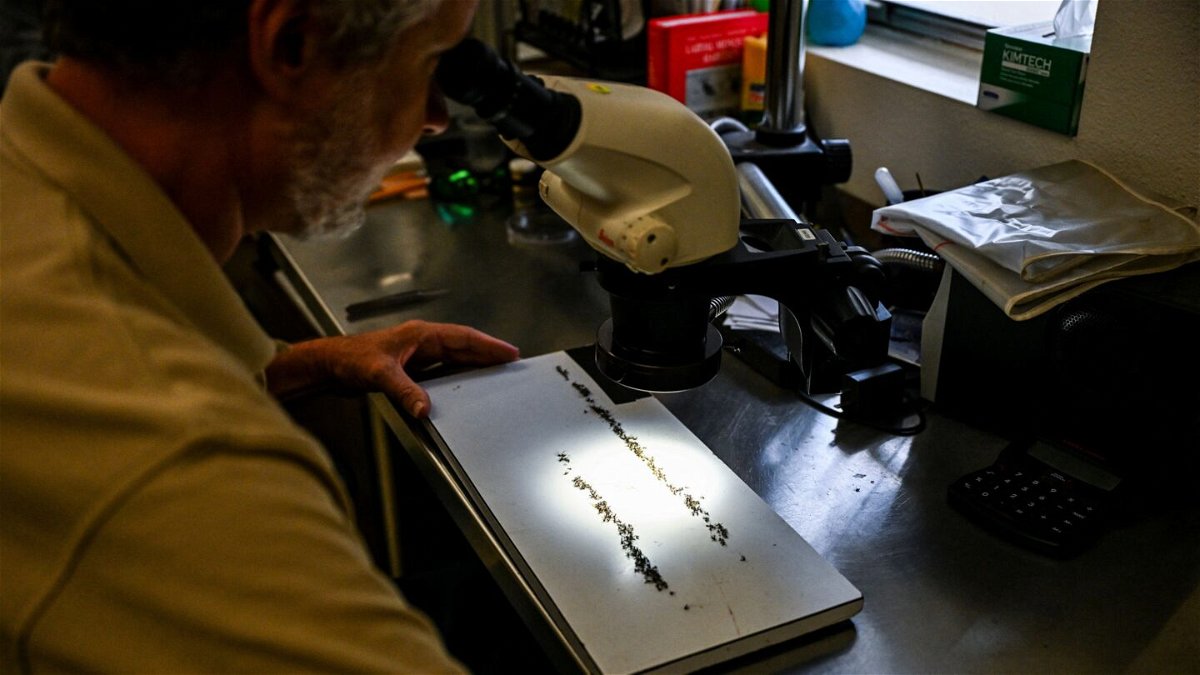
In Sarasota County, Florida, where seven of the eight locally acquired cases were identified this summer, containing malaria is still a matter of targeting the mosquitoes, both as adults and in the larval stage. Mosquito control teams say they have sprayed more than 470 miles with pesticides targeted at adult mosquitoes using trucks at night and have targeted swamps and canals with so-called larvicides to stop them earlier in their life cycle.
One major difference in control efforts now compared with 70 years ago: Then, work also included spraying indoor surfaces of homes with insecticide, in particular DDT, Markowski said — a chemical rarely used now because of harmful health and environmental impacts.
“DDT was the standard for quite a while,” Markowski said. Applications indoors, as well as outside using trucks and aircraft, “suppressed the mosquito population enough that they were able to eliminate malaria.”
But because anopheles mosquitoes persist in the US, so does the risk for transmission. And every year, about 2,000 cases of travel-related malaria are diagnosed in the US, the CDC says.
Before this summer, local transmission hadn’t been detected since 2003, when eight cases were found in Palm Beach County, Florida, a track record that the CDC’s McElroy attributes in part to strong case detection.
“When persons do come back from a country where malaria is transmitted and they start to develop symptoms, they present to the health care system,” he said. “That case is diagnosed and ultimately treated, and that case is then reported initially to the county health department and state health department and ultimately to CDC.”
It can be difficult for a US health care provider to know to suspect malaria; its symptoms include fever, chills, headache and fatigue. The plasmodium parasites that cause it infect liver cells and red blood cells, and the disease can be treated with medicines that kill them.
If not treated promptly, malaria can cause severe disease. Every year before the Covid-19 pandemic, about 300 people in the US developed severe malaria, and five to 10 people died each year, according to CDC data.
It takes a few things to happen to consider a local malaria outbreak over, the CDC says: The most recent patient treated no longer has parasites in their system capable of infecting a mosquito, any mosquito possibly infected by that patient has died, and no new patient has been detected. All told, that’s usually about eight to 10 weeks after treatment is completed.
And while tools are better now, the AMCA’s Markowski said there are a few things that may make it harder to combat malaria: Modern mosquito control is typically a very local effort, very strong in states like Florida and New Jersey, he said, and “more of a hodgepodge” in others. This is not at all like the federal effort mounted in the 1940s.
Markowski also suggested that increased skepticism around public health efforts, particularly after the Covid pandemic, presents a new hurdle.
“One of our biggest challenges is how to convince people that we’re trying to help and it’s in all of our best interest if we have disease-free lives and can enjoy the world that we live in,” Markowski said.
Still, he and other experts said local malaria transmission doesn’t pose a major public health threat in the US.
“In the States, what worries more people are viral infections,” the NIH’s Barillas-Mury said. “Zika or dengue, things like that.”
Against those diseases, spread by mosquitoes called Aedes aegypti and Aedes albopictus, approaches include more newfangled technologies similar to the Delftia bacteria work published this month in Science.
Verily, part of Google owner Alphabet, has a project called Debug that uses a bacteria called Wolbachia in male mosquitoes that renders them unable to have offspring.
A company called Oxitec rears male mosquitoes with a “self-limiting gene” that prohibits offspring from surviving to adulthood. Both approaches use male mosquitoes because they don’t bite. Oxitec also says it’s working on applying the approach to anopheles mosquitoes for malaria control as well.
The Delftia bacteria approach still needs to go through further testing, Barillas-Mury said, but she noted that it potentially contributes to more tools than ever to make a dent in the toll of malaria.
“We’ve come a long way,” she said. “I’m more optimistic than ever; it seemed absolutely impossible when I started 30 years ago … but I think now we have many more options. And I think they’re all coming together.”
The-CNN-Wire
™ & © 2023 Cable News Network, Inc., a Warner Bros. Discovery Company. All rights reserved.






