Understanding premenstrual dysphoric disorder, its causes, symptoms, and effective management

Yuri A // Shutterstock
Understanding premenstrual dysphoric disorder, its causes, symptoms, and effective management
woman curled up on couch from pain
What is premenstrual dysphoric disorder (PMDD)?
Many women dread the mild-to-moderate physical and emotional symptoms that come before that time of the month. But those with premenstrual dysphoric disorder (more commonly referred to as PMDD) encounter these symptoms at intensities reaching the extremes where they can significantly affect their quality of life. So if this sounds like you, perhaps your monthly symptoms are not as normal as you thought.
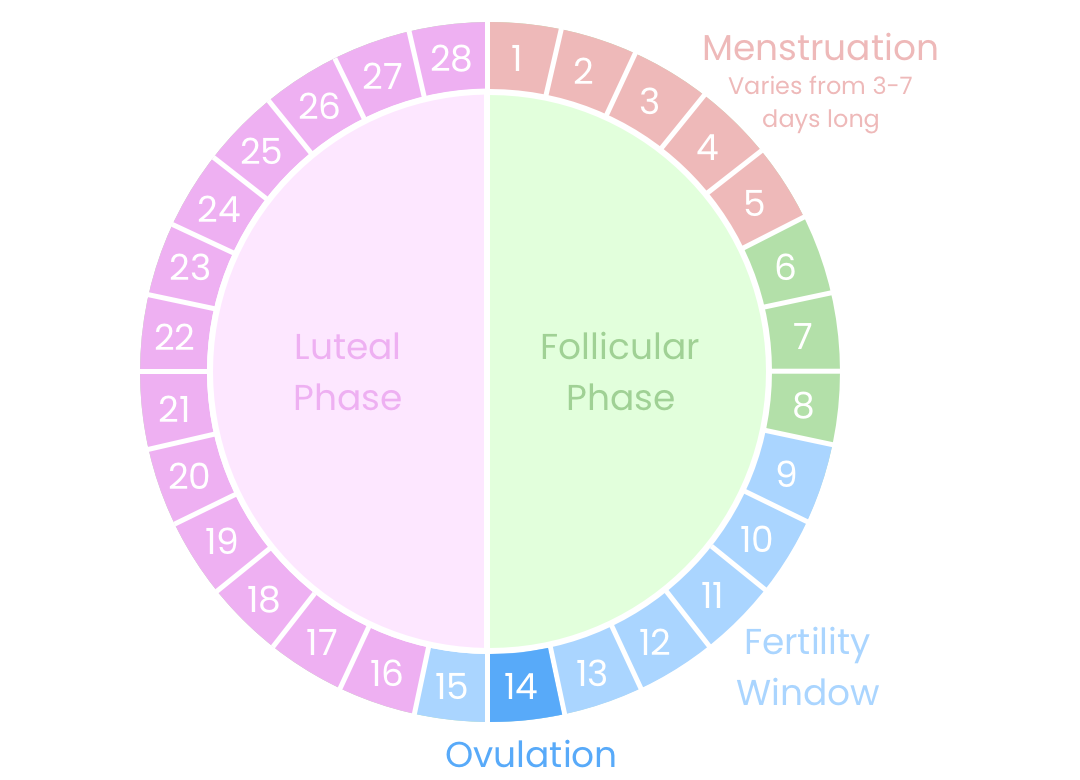
Occurring during the luteal phase of the menstrual cycle (the time between ovulation and the start of menstruation), PMDD is a condition caused by your body’s response to normal hormone changes before your menstrual period. Currently, PMDD is recorded to affect between 3% and 8% and is estimated to affect between 13% and 18% of all people who menstruate.
Guava Health walks you through premenstrual dysphoric disorder, its causes, symptoms, and how to plan for effective management post-diagnosis.
![]()
Guava Health
What are the symptoms of PMDD?
diagram showing phases of menstrual cycle within 28 days
PMDD can present itself in various ways, and the symptoms can vary from person to person. These symptoms typically occur in the week or two before menstruation and go away after the onset of menstruation. Some common ways in which PMDD may present itself include:
Emotional symptoms: Intense mood swings, increased sensitivity to rejection, feelings of sadness or hopelessness, frequent crying spells, irritability, anger, increased conflicts with others, anxiety or tension.
Behavioral symptoms: Social withdrawal, difficulty concentrating, less interest in usual activities or relationships, feeling overwhelmed or out of control, changes in appetite (food cravings or overeating), sleep issues (insomnia or excessive sleep).
Physical symptoms: Breast tenderness or swelling, bloating or weight gain, headaches or migraines, joint or muscle pain, fatigue, or lack of energy.
How do I know I have PMDD and not another condition?
Currently there are no tests capable of diagnosing PMDD directly, though blood or saliva tests can be helpful in ruling out other underlying disorders. The primary method for diagnosing PMDD is through the daily tracking of symptoms over a minimum of two menstrual cycles.
Additionally, this condition presents distinct diagnostic challenges for healthcare professionals because the symptoms and psychological nature of PMDD look similar to other mental health conditions like depression and bipolar disorder.
Furthermore, the formal recognition of PMDD as a legitimate diagnosis occurred relatively recently. As a result, numerous healthcare providers lack training in PMDD, often struggling to know where to start when it comes to treating the condition.
Getting real about PMDD: Jen Ruggirello’s personal struggle
Jen Ruggirello, former Buzzfeed video producer and host of the Kitchen and Jorn Show, recently shared that she was diagnosed with PMDD. Prior to her diagnosis, Ruggirello thought her feelings of “suicidal ideation” and “two weeks of just depression” was an experience similar to that of “everyone, like this is normal.” This meant that every cycle she would “have to take my monthly two-week vacation of misery.”
In retrospect, Ruggirello stated that “you don’t realize until you’re not depressed anymore how much depression takes from you” and expressed that she feels that she “got a lot of my life back” post-diagnosis and treatment.
What can I do to make my PMDD more manageable?
With many options available, effectively addressing PMDD symptoms can significantly enhance the quality of life for those affected. Below are some commonly recommended strategies for managing PMDD:
Tracking symptoms: While each person may experience PMDD differently, keeping track of your symptoms can better prepare you for upcoming feelings and be a good reference during medical appointments. If you’re uncertain about what to jot down, here is a comprehensive collection of the most common symptoms.
Medications: Many patients with PMDD find relief through the use of antidepressants that slow the reuptake of serotonin. Another option is Vitex, an herbal remedy that supports natural hormone balance through stimulation of certain bodily systems. Recent studies found Vitex to be notably effective in diminishing the physical symptoms of PMDD. Note that it is always advisable to consult with a medical professional prior to starting any medication.
Hormonal interventions: Combined oral contraceptives or other forms of hormonal birth control can aid some people in regulating hormone levels, thereby reducing the intensity of PMDD symptoms.
Lifestyle modifications: Doing regular exercise, getting enough sleep, eating well, and doing calming activities like deep breathing can also help.
Moving forward with PMDD
By recognizing PMDD symptoms and taking action, you can enhance your quality of life and advocate for better understanding of this disorder within the medical community. Since most people typically experience around 450 periods in their lifetime, PMDD is a chronic condition requiring long-term management.
This story was produced by Guava Health and reviewed and distributed by Stacker Media.






